The specter of antibiotic resistance looms large over modern medicine, a silent pandemic unfolding in hospitals and communities worldwide. For decades, these miracle drugs have served as the bedrock of our defense against bacterial infections, turning once-lethal diseases into manageable conditions. Yet this golden era is under threat. Bacteria, in their relentless drive for survival, have evolved sophisticated mechanisms to evade the very compounds designed to kill them. The relentless selection pressure exerted by the widespread—and often inappropriate—use of antibiotics has accelerated this evolutionary arms race, pushing us toward a precarious future where common infections could once again become deadly.
The development of novel antibacterial agents is no longer a mere scientific pursuit; it is an urgent global health imperative. The pipeline, however, is fraught with immense scientific and economic challenges. The low-hanging fruit has long been picked. Discovering entirely new classes of antibiotics with novel mechanisms of action that can bypass existing resistance pathways is a monumental task. Furthermore, the economic model for antibiotic development is broken. These are typically short-course therapies, and the most potent new agents are often held in reserve as drugs of last resort, limiting their commercial viability. This has led many large pharmaceutical companies to exit the field, leaving the future of discovery in the hands of smaller biotech firms and academic consortia.
In response to this crisis, the scientific community is pioneering a multifaceted arsenal of innovative strategies. One promising frontier involves the exploration of natural products from untapped ecological niches. Extreme environments, from the depths of the ocean to volcanic springs, harbor microbes that produce unique chemical weapons in their own battles for survival. By employing advanced metagenomics and synthetic biology, researchers can now access and engineer these cryptic genetic pathways to produce novel compounds that bacteria have never encountered.
Another groundbreaking approach is the targeted design of narrow-spectrum antibiotics. Moving away from the traditional broad-spectrum "kill everything" model, these precision medicines are designed to target specific, essential pathways in a particular pathogen. This strategy minimizes collateral damage to the beneficial microbiome, which is crucial for human health and helps reduce the development of resistance. This requires sophisticated diagnostics to rapidly identify the causative pathogen, driving a synergistic partnership between therapeutics and diagnostics.
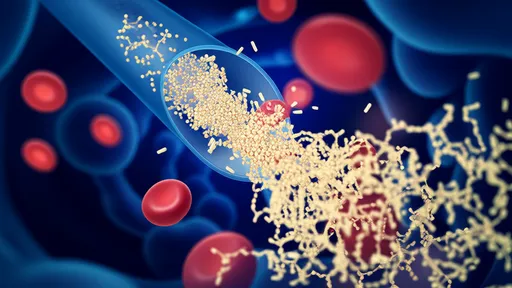
Beyond small molecules, scientists are venturing into entirely new therapeutic modalities. Antibody-antibiotic conjugates represent a clever fusion of biologic and chemical technology. These sophisticated drugs use a pathogen-specific antibody as a homing device to deliver a potent antibiotic payload directly to the bacterial cell, sparing healthy human cells and drastically increasing the local concentration of the drug at the site of infection.
The field of phage therapy, the use of viruses that specifically infect and kill bacteria, is also experiencing a major renaissance. Once a curiosity from the Soviet era, bacteriophages are now being rigorously studied in Western medicine. Their key advantage is their ability to co-evolve with their bacterial hosts, potentially overcoming resistance. Researchers are engineering phages to enhance their killing power and to disrupt the bacterial biofilms that often shield communities of bacteria from conventional antibiotics.
Perhaps the most futuristic approaches involve disarming the pathogen rather than killing it. Strategies focused on anti-virulence factors aim to neutralize the toxins and other molecules bacteria use to cause disease. By rendering the bacteria harmless, this approach removes the selective pressure that drives resistance, as the bacteria can live without necessarily developing defenses. Similarly, research into lytic enzymes that specifically break down bacterial cell walls offers a direct and potentially resistance-proof method of killing.
Despite these exciting scientific breakthroughs, the path from the laboratory to the patient is long and perilous. Revitalizing the antibiotic pipeline requires a fundamental reshaping of the economic landscape. Public-private partnerships, such as the Combating Antibiotic-Resistant Bacteria Biopharmaceutical Accelerator (CARB-X), and new subscription-style payment models, like those being piloted in the UK, are critical steps. These models de-link the reward for innovation from the volume of drug sales, incentivizing companies to develop new antibiotics based on their value to public health rather than their market potential.
The battle against antibiotic resistance is a race against time. It demands a concerted, global effort that marries cutting-edge science with sustainable economic policies and robust stewardship programs to preserve the efficacy of new drugs once they arrive. The development of novel antimicrobials is not just about discovering new molecules; it is about safeguarding the very foundation of modern medicine for generations to come. The ingenuity on display in laboratories around the world offers a beacon of hope, but realizing that potential will require unwavering commitment from all sectors of society.

By /Aug 25, 2025

By /Aug 25, 2025

By /Aug 25, 2025

By /Aug 25, 2025

By /Aug 25, 2025

By /Aug 25, 2025
By /Aug 25, 2025

By /Aug 25, 2025

By /Aug 25, 2025
By /Aug 25, 2025

By /Aug 25, 2025

By /Aug 25, 2025

By /Aug 25, 2025

By /Aug 25, 2025

By /Aug 25, 2025

By /Aug 25, 2025

By /Aug 25, 2025

By /Aug 25, 2025

By /Aug 25, 2025

By /Aug 25, 2025