In the evolving landscape of medical science, the application of gene therapy for rare diseases represents one of the most groundbreaking advancements of the 21st century. Rare diseases, often caused by specific genetic mutations, have long posed significant challenges due to their low prevalence and the consequent lack of targeted treatments. For decades, patients and clinicians faced limited options, relying mostly on symptomatic management rather than addressing the root cause. However, the emergence of gene therapy has begun to rewrite this narrative, offering hope where there was once resignation.
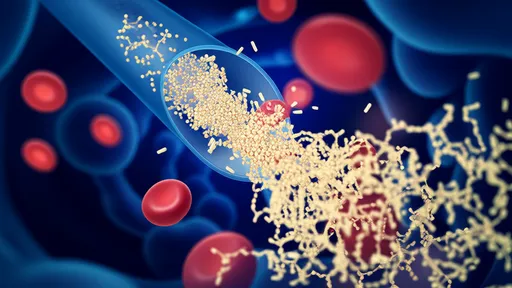
The core premise of gene therapy lies in its ability to deliver functional genes to compensate for defective ones, effectively correcting the underlying genetic anomalies responsible for these conditions. This approach marks a paradigm shift from traditional pharmacotherapy, which typically focuses on managing symptoms or slowing disease progression. Instead, gene therapy aims for a potential one-time treatment that could provide long-term or even permanent benefits. The development of viral vectors, such as adeno-associated viruses (AAVs), has been instrumental in this progress, enabling efficient and targeted delivery of therapeutic genes to specific cells or tissues.
One of the most celebrated successes in this domain is the treatment of spinal muscular atrophy (SMA), a devastating neuromuscular disorder caused by mutations in the SMN1 gene. The approval of onasemnogene abeparvovec, a gene therapy drug, has transformed outcomes for infants diagnosed with SMA. Clinical trials demonstrated remarkable improvements in motor function and survival, with many patients achieving milestones previously thought unattainable. This therapy works by delivering a functional copy of the SMN1 gene via an AAV vector, effectively halting motor neuron degeneration and promoting neuronal health.
Similarly, gene therapy has shown promising results in addressing inherited retinal diseases, such as Leber congenital amaurosis (LCA). Mutations in the RPE65 gene lead to progressive vision loss and blindness in affected individuals. The introduction of voretigene neparvovec, an AAV-based gene therapy, has enabled the production of functional RPE65 protein in retinal cells, restoring visual function in many patients. Clinical studies reported significant improvements in light sensitivity, visual fields, and navigational abilities, fundamentally enhancing the quality of life for those living with this condition.
Beyond these examples, gene therapy is being explored for a wide array of other rare genetic disorders, including hemophilia, lysosomal storage diseases, and certain metabolic conditions. In hemophilia, for instance, experimental therapies aim to introduce functional clotting factor genes, reducing or eliminating the need for frequent intravenous infusions. Early results have been encouraging, with some patients maintaining stable factor levels years after treatment. This not only alleviates the burden of disease but also reduces the risk of complications associated with traditional treatments.
Despite these advancements, the clinical application of gene therapy is not without challenges. Safety remains a paramount concern, particularly regarding immune responses to viral vectors and the potential for unintended genetic modifications. Cases of hepatotoxicity and neuroinflammation have been reported in some trials, underscoring the need for rigorous monitoring and tailored immunosuppressive strategies. Moreover, the long-term effects of gene therapy are still being studied, as many approved treatments have relatively short follow-up periods. Continuous research is essential to fully understand the durability of therapeutic effects and any delayed adverse events.
Another significant hurdle is the accessibility and affordability of these treatments. Gene therapies are among the most expensive medical interventions ever developed, with costs often running into millions of dollars per patient. This poses ethical and economic dilemmas for healthcare systems worldwide, raising questions about equitable access and sustainable financing. Efforts are underway to develop innovative payment models, such as outcome-based agreements and installment plans, to mitigate financial barriers and ensure that breakthroughs benefit a broader population.
Looking ahead, the future of gene therapy for rare diseases appears increasingly promising. Advances in vector engineering, such as the development of novel capsids with enhanced tropism and reduced immunogenicity, are poised to improve the safety and efficacy of these treatments. Additionally, emerging technologies like CRISPR-Cas9 offer the potential for more precise genetic corrections, moving beyond gene addition to actual gene editing. These innovations could expand the scope of treatable conditions and enhance the precision of therapeutic interventions.
In conclusion, gene therapy has undeniably revolutionized the treatment landscape for rare genetic diseases, offering curative potential where few options existed. From SMA to inherited blindness, these therapies have demonstrated transformative outcomes, bringing hope to patients and families worldwide. However, overcoming challenges related to safety, accessibility, and cost will be crucial for maximizing their impact. As research continues to advance, the integration of gene therapy into mainstream medicine promises to redefine the standards of care for rare diseases, embodying the true spirit of precision medicine.

By /Aug 25, 2025

By /Aug 25, 2025

By /Aug 25, 2025

By /Aug 25, 2025

By /Aug 25, 2025

By /Aug 25, 2025
By /Aug 25, 2025

By /Aug 25, 2025

By /Aug 25, 2025
By /Aug 25, 2025

By /Aug 25, 2025

By /Aug 25, 2025

By /Aug 25, 2025

By /Aug 25, 2025

By /Aug 25, 2025

By /Aug 25, 2025

By /Aug 25, 2025

By /Aug 25, 2025

By /Aug 25, 2025

By /Aug 25, 2025